

This will also manifest as a junctional escape rhythm on the ECG. In such scenarios, cells in the bundle of His (which possess automaticity) will not be reached by the atrial impulse and hence start discharging action potentials and an escape rhythm. For example, consider a complete block located in the atrioventricular node. If there are cells (with automaticity) distal to the block, an escape rhythm may arise in those cells. During complete heart block (third-degree AV-block) the block may be located anywhere between the atrioventricular node and the bifurcation of the bundle of His.

In case of sinus arrest (or any scenario in which atrial impulses do not reach the atrioventricular node), junctional escape rhythm may be life-saving. Junctional escape rhythm is a regular rhythm with a frequency of around 40–60 beats per minute. Three or more consecutive junctional beats are referred to as junctional rhythm (also called junctional escape rhythm). Less than three consecutive beats are referred to as junctional beats (also called junctional escape beats). If the normal sinus impulse disappears (e.g sinus arrest) cells around the atrioventricular node may discharge impulses.Junctional rhythm may arise in the following situations: If the ventricles are activated prior to the atria, a retrograde P-wave (leads II, III and aVF) will be seen after the QRS complex.
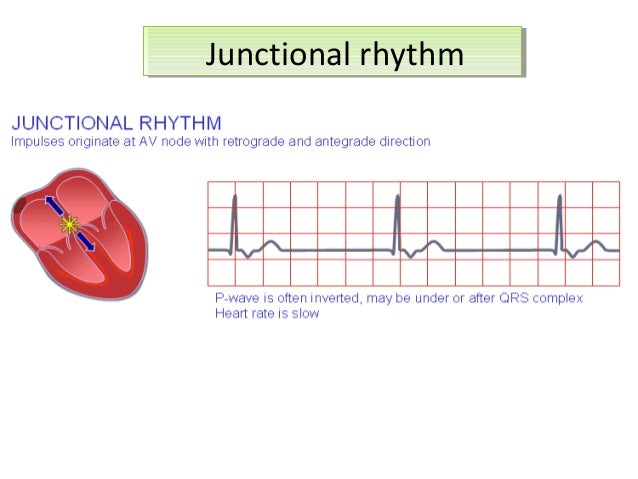
If the atria are activated prior to the ventricles, a retrograde P-wave will be visible in leads II, III and aVF prior to the QRS complex. In most cases, the P-wave is not visible because when impulses are discharged from the junctional area, atria and ventricles are depolarized simultaneously and ventricular depolarization (QRS) dominates the ECG. The atria will be activated in the opposite direction, which is why the P-wave will be retrograde. In both cases listed above the impulse will originate in the junction between the atria and the ventricles, which is why ectopic beats and ectopic rhythms originating there are referred to as junctional beats and junctional rhythms.


 0 kommentar(er)
0 kommentar(er)
